- How Are Ulcers Formed from Drinking Alcohol?
- Alcohol Treatment, Recovery & Sobriety Stories
- Fibromyalgia & Alcohol Use: Does Drinking Cause Muscle Pains & Aches?
- MAST Assessment: The Michigan Alcohol Screening Test (25 Questions)
- Living With an Alcoholic: How to Deal With an Alcoholic Spouse
- Alcohol & Dementia: Can Alcohol
- Cause Memory Loss?
- Delirium Tremens: Symptoms, Timeline & Treatment
- Stages of Alcoholism: Early, Chronic and End Stage
- Alcohol Shakes & Tremors: When Do I Need Professional Help?
- Children of Alcoholics: Growing Up with an Alcoholic Parent
Alcohol Addiction & Abuse: Signs, Symptoms, and Treatment
Last Medical Review on: August 21, 2023 Updated: May 16, 2024
Alcohol addiction, clinically referred to as alcohol use disorder (AUD), is a common, chronic, and sometimes-progressive medical condition that involves the compulsive consumption of alcohol. Maladaptive patterns of drinking can lead to several serious social, familial, and physical consequences. Fortunately, there are highly effective and diverse alcohol use treatment programs available to people with mild-to-severe AUDs.
What you will learn
- Effects of alcohol use
- Signs of alcohol overdose
- Symptoms of alcohol addiction
- Methods used to treat alcohol addiction
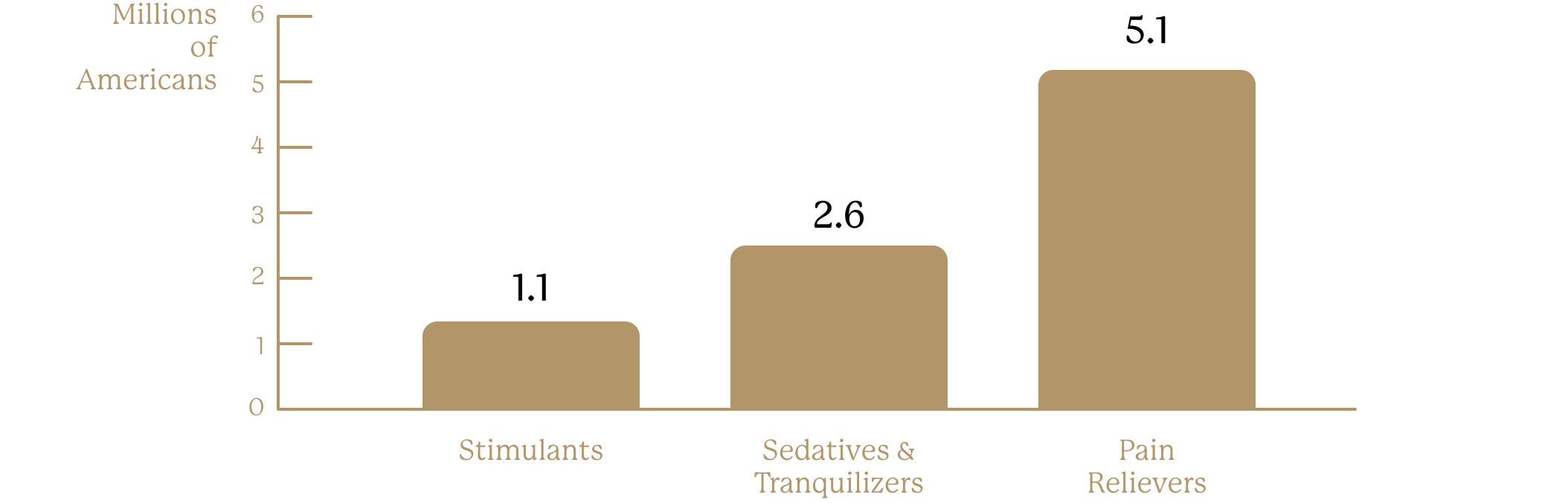
~7.0 Million Americans Reported Past-Month Use of Rx Drugs for Non-medical Purposes in 2010
Sources
Office of Applied Studies, Substance Abuse and Mental Health Services Administration, National Survey on Drug Use and Health, 2010
Am I Addicted to Alcohol?
Besides the DSM-5, healthcare professionals might utilize other tools to assess your alcohol use and the severity of an AUD.7 That’s why it’s important to talk honestly to your healthcare provider, who can give you a thorough evaluation and diagnosis.
Additionally, there are many tools you can find online to help you examine the nature of your alcohol use and your behaviors surrounding it. In fact, we have one. It’s important to note that our “Has My Alcohol Use Become a Problem?” questionnaire is intended for educational purposes and should not be used to self-diagnose. This evaluation is not a substitute for advice from a medical doctor.
Take our free, 5-minute alcohol use self-assessment below if you think you or someone you love might be struggling with alcohol misuse. This evaluation consists of 11 yes or no questions that are designed to be used as an informational tool to assess the severity and probability of an alcohol use disorder. The test is free, confidential, and no personal information is needed to receive the result.
Alcohol also affects more than just the mind. Evidence indicates that long-term alcohol use increases an individual’s risk of developing certain cancers and cardiovascular conditions such as high blood pressure, heart disease, and stroke. It can also damage the liver, lead to pancreatitis, and weaken the immune system.8,9
Additionally, chronic alcohol use can lead to dependence—wherein the body becomes so used to having alcohol present that without it, potentially dangerous withdrawal symptoms surface. It can also result in addiction.8
What are the Causes of Alcohol Addiction?
Some of a person’s risk in developing an AUD depends on how much, how often, and how quickly they consume alcohol. Certain biological, psychological, and social influences are also believed to play a role in the development of AUDs. Some risk factors that may lead to someone developing an AUD can include:1,10
- Genetics.
- A family history of alcohol use disorder.
- Parental drinking patterns.
- Exposure to trauma and stress during childhood.
- Drinking alcohol at an early age. Scientists have found that people who began drinking at age 15 or younger were
- 5 times more likely to develop an AUD than those who started drinking at age 21 or older. In addition, the risk
- for women among this group is higher than for men.
Certain psychiatric disorders, including major depression, bipolar disorder, anxiety disorders, and antisocial personality disorder are commonly associated with alcohol use disorder, although whether or not these co-occurring disorders are a result of alcohol use disorder or contributed to the development of an alcohol use disorder is unclear and may differ for each individual. Some studies suggest that schizophrenia, depression, and personality disorders are also predisposing factors for AUDs. This means that if a person has one or more of these psychiatric conditions, they may have an increased risk of alcohol use disorder.11
Alcohol Addiction Treatment
Although there is currently no cure for alcohol use disorders, AUDs—much like many other chronic, relapsing diseases—can be successfully managed and treated.1 Professional addiction treatment in a rehabilitation center can help people suffering with AUDs recover from substance misuse issues and remain sober. If you or someone you care about is struggling with an AUD, you will likely benefit from some form of treatment.
If you’re considering professional addiction treatment for problematic alcohol use, you have a variety of options to treat your AUD, ranging from detoxification, to inpatient and outpatient rehabilitation, behavioral therapies, medication, and mutual-help groups.1
Effects of Alcohol Addiction on Your Health
Repeated, prolonged alcohol use impacts an individual’s physical and mental health. It is associated with cognitive and mental health issues, including learning and memory problems as well as worsening or causing mental health conditions like depression and anxiety.7
Alcohol also affects more than just the mind. Evidence indicates that long-term alcohol use increases an individual’s risk of developing certain cancers and cardiovascular conditions such as high blood pressure, heart disease, and stroke. It can also damage the liver, lead to pancreatitis, and weaken the immune system.8,9
Additionally, chronic alcohol use can lead to dependence—wherein the body becomes so used to having alcohol present that without it, potentially dangerous withdrawal symptoms surface. It can also result in addiction.8
What are the Causes of Alcohol Addiction?
Some of a person’s risk in developing an AUD depends on how much, how often, and how quickly they consume alcohol. Certain biological, psychological, and social influences are also believed to play a role in the development of AUDs. Some risk factors that may lead to someone developing an AUD can include:1,10
- Genetics.
- A family history of alcohol use disorder.
- Parental drinking patterns.
- Exposure to trauma and stress during childhood.
- Drinking alcohol at an early age. Scientists have found that people who began drinking at age 15 or younger were
- 5 times more likely to develop an AUD than those who started drinking at age 21 or older. In addition, the risk for women among this group is higher than for men.
Certain psychiatric disorders, including major depression, bipolar disorder, anxiety disorders, and antisocial personality disorder are commonly associated with alcohol use disorder, although whether or not these co-occurring disorders are a result of alcohol use disorder or contributed to the development of an alcohol use disorder is unclear and may differ for each individual. Some studies suggest that schizophrenia, depression, and personality disorders are also predisposing factors for AUDs. This means that if a person has one or more of these psychiatric conditions, they may have an increased risk of alcohol use disorder.11
Take the first step
towards recovery
Our representatives are standing
by 24-7 to help you start healing today
Alcohol Detoxification
Detox is an ideal first step toward recovery from an AUD, but detox alone is rarely sufficient in helping a person achieve long-term abstinence.12 Detoxification is a set of interventions designed to help someone safely and comfortably withdraw from alcohol, which then positions them to transition into a formal, potentially longer treatment program.
Before entering a detoxification center, a physician will need to perform a thorough assessment of a patient’s experience with alcohol misuse, previous withdrawal experiences (if any), and their medical and psychiatric history in order to determine their withdrawal risk. For the sake of this assessment, patients may also undergo blood tests and screening for the presence of any co-occurring mental or physical health issues.
Individuals at risk of severe, life-threatening withdrawal symptoms, including seizures and delirium tremens (DTs), should undergo detox in an inpatient facility, such as a hospital or other acute care facility, according to the Substance Abuse and Mental Health Services Administration (SAMHSA).2ve an increased risk of alcohol use disorder.11
Residential or Inpatient Alcohol Rehab
Inpatient or residential AUD treatment entails patients living and residing in the rehabilitation center 24/7. Inpatient alcohol rehab may vary in duration, sometimes consisting of short stays of 3–6 weeks, which may or may not be followed by attendance at an outpatient rehab. Some people require longer stays of 6–12 months at facilities known as therapeutic communities (TCs), which provide structured programming and offer assistance with reintegration into their community.
Inpatient and residential rehab stays are beneficial because they remove a person from distractions and environments where they may be surrounded by people, places, or events that can trigger a relapse, allowing them to focus solely on their recovery and building the necessary coping skills to live a sober life. Here, patients also receive around-the-clock care and monitoring, which helps address any post-acute withdrawal symptoms and offers necessary support.12
Alcohol Detox Medications
- Benzodiazepines, such as diazepam, chlordiazepoxide, oxazepam, or lorazepam. Administering benzodiazepines early during alcohol withdrawal may help reduce the severity of withdrawal symptoms, preventing a progression to potentially serious and fatal consequences.
- Anticonvulsants like carbamazepine, gabapentin, or topiramate. These medications help reduce drinking behavior and treat mild-to-moderate withdrawal symptoms. Topiramate has not yet received approval from the U.S. Food and Drug Administration (FDA) but has shown promise in treating alcohol addiction.
- Antipsychotics, like haloperidol, which can reduce extreme agitation, hallucinations, delusions, and delirium during alcohol withdrawal.
Alcoholism Aftercare and Long-Term Health
Recovery from alcohol addiction is a lifelong process that does not end when addiction treatment completes. After finishing a rehabilitation program, many people choose to participate in some form of aftercare. Many of the aftercare methods below are extensions of similar or even the same types of therapy a person receives in primary treatment. Aftercare is the word used to describe long-term, ongoing treatment that begins once intensive forms of rehabilitation end and is designed to provide additional support and help prevent relapse.17 Patients may choose to participate in one or many different types of aftercare, such as:17
- A stay at a therapeutic community (TC), where patients can live with others who are in recovery as a way of gaining support as they re-enter sober daily life.
- Individual counseling to help patients develop insight into the issues that can lead to relapse, and learn alternative coping mechanisms so they do not return to drinking.
- Group therapy, which is led by a counselor and includes others in recovery.
- Mutual-help groups, such as 12-step groups like Alcoholics Anonymous (AA) or non-12 step groups like SMART Recovery.
- Complementary or alternative treatments, such as art therapy or music therapy, which are typically beneficial for people who are also participating in another form of aftercare.
- Couples or family counseling can help address underlying issues and continue to work on the relationship.
Alcohol addiction
treatment FAQS
About the Contributor
Hilary Curtis
Dr. Curtis has a depth of experience in providing trauma-informed treatment for mental health and substance use issues with adolescents and adults, and intensive experience with criminal justice populations where...
Read Our Editorial PolicyRelated Topics
Sources
[1] Florida Department of Law Enforcement. (n.d.). Drugs in deceased persons. Retrieved from https://www.fdle.state.fl.us/MEC/Publications-and-Forms/Documents/Drugs-in-Deceased-Persons on April 30, 2023
[2] Centers for Disease Control and Prevention. (2022, April 29). Florida priority topic investments. Retrieved from https://www.cdc.gov/injury/budget/policystatesnapshots/Florida.html on April 30, 2023
[3] Jegede O;Rhee TG;Stefanovics EA;Zhou B;Rosenheck RA; (n.d.). Psychiatry research. Rates and correlates of dual diagnosis among adults with psychiatric and substance use disorders in a nationally representative U.S sample. Retrieved from https://pubmed.ncbi.nlm.nih.gov/35834863/ on April 30, 2023






